Role: UX Researcher/Product Designer
Scope: End-to-end ownership: research, interaction design, prototyping, validation, and deployment. All design decisions made independently and validated with clinicians.
Context
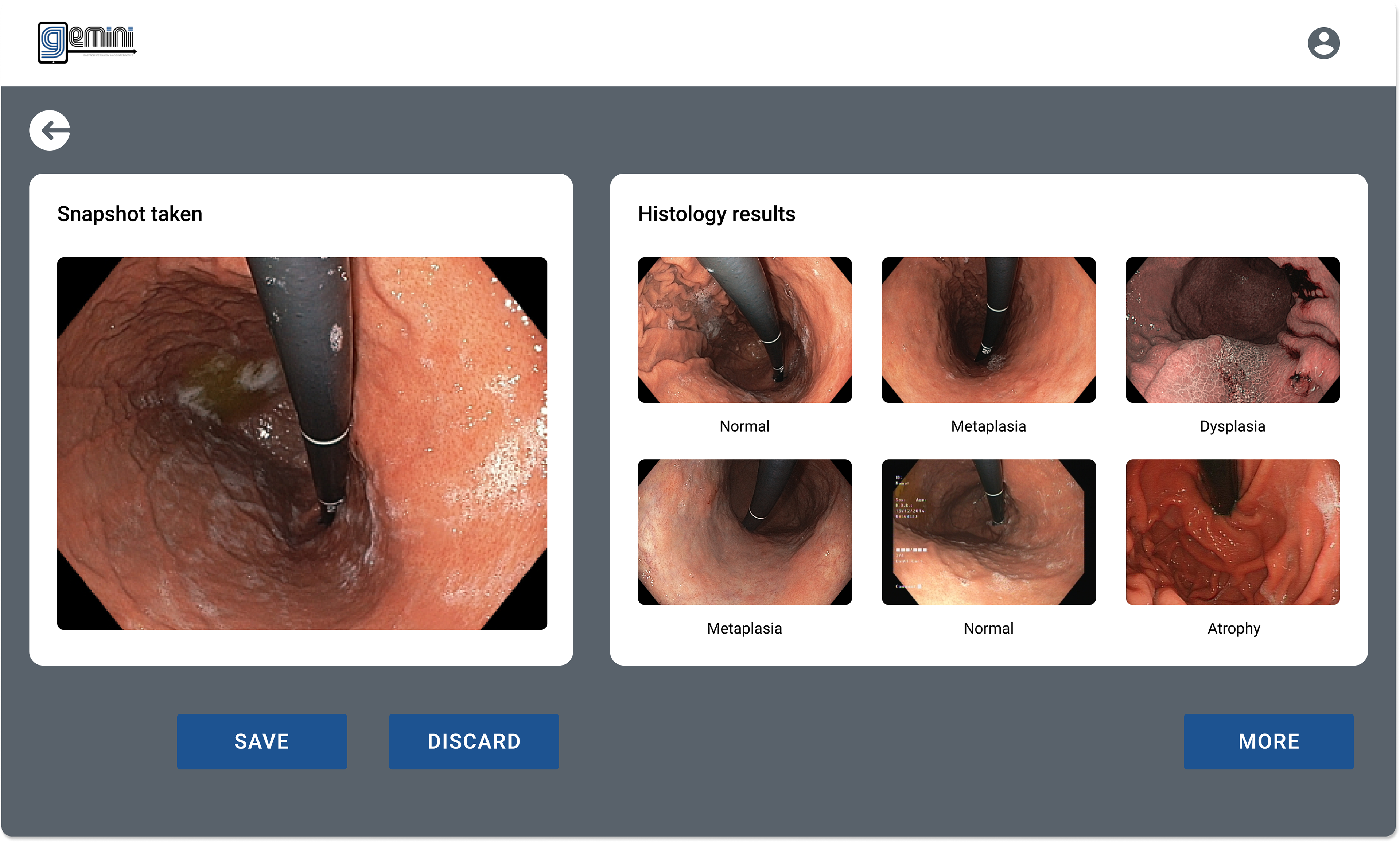
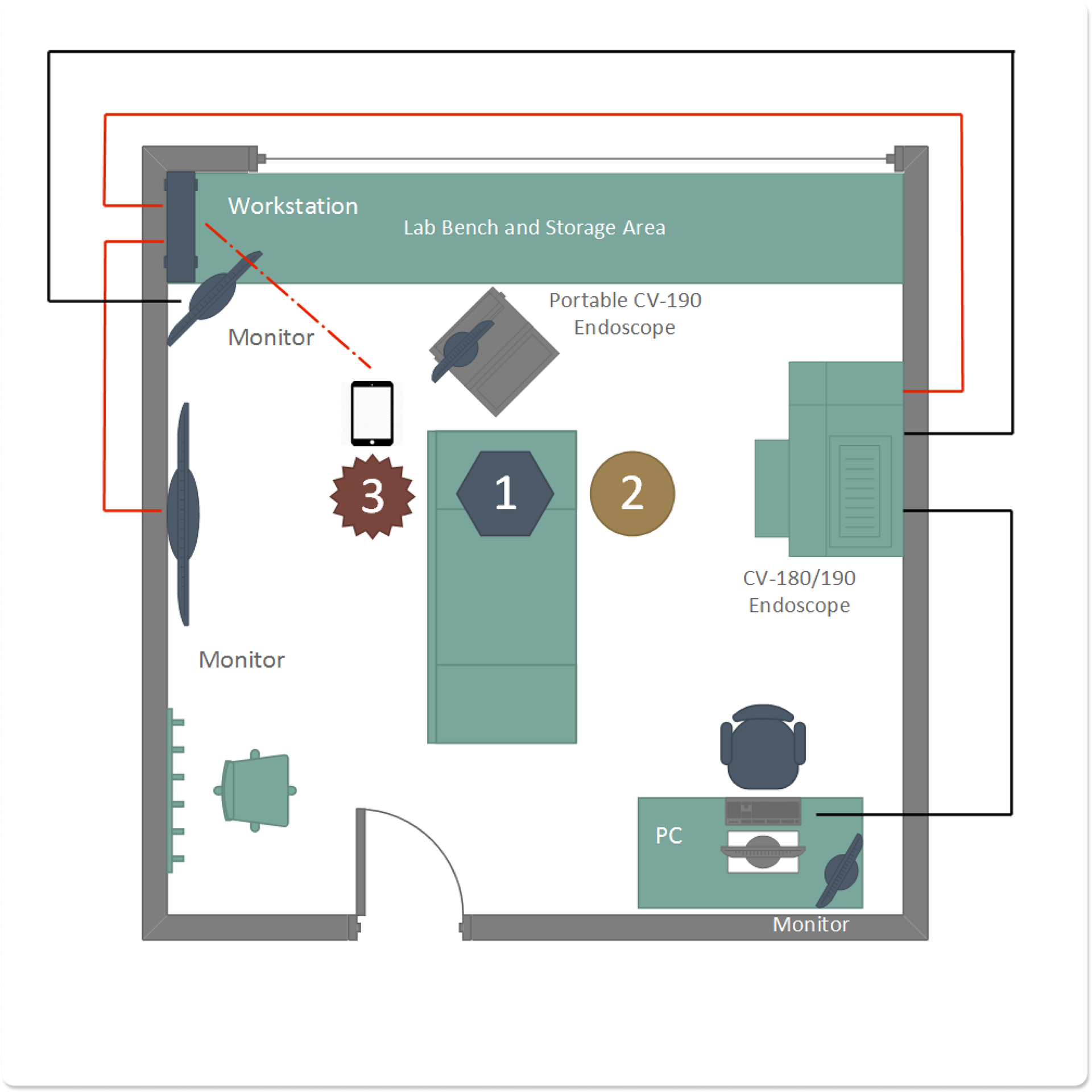
GEMINI was a computer-assisted clinical decision support system designed to support gastroenterologists during live endoscopic examinations. It was developed as part of a novel diagnostic protocol for premalignant gastric conditions and deployed across multiple medical centers in Europe.
The environment imposed strict constraints: procedures were live, clinicians’ hands and visual attention were fully occupied, and existing workflows and equipment could not be altered.
The Problem
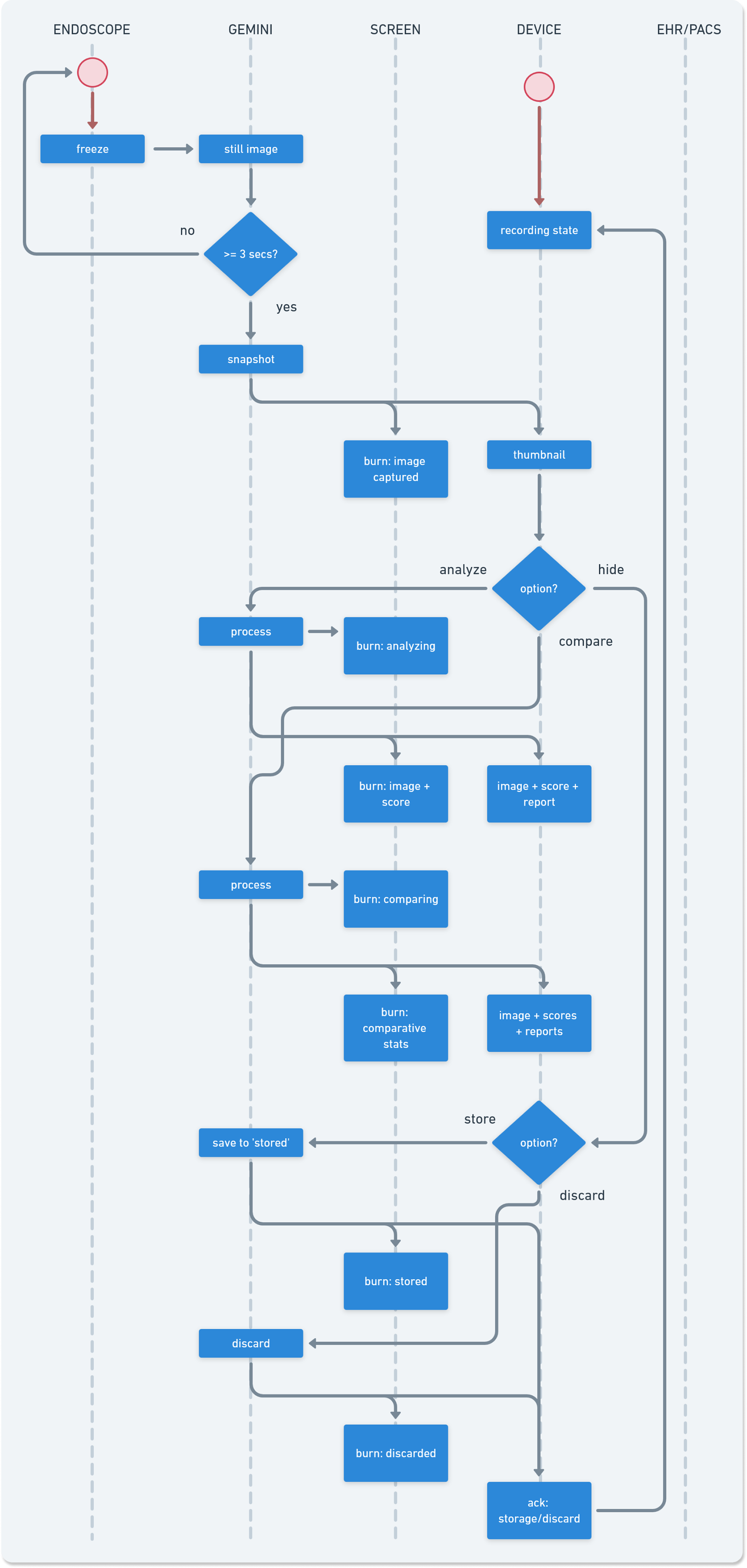
Clinicians needed real-time decision support without disrupting procedural flow, attention, or patient safety. Most existing digital tools assumed post-procedure analysis or interaction models incompatible with sterile, time-critical clinical settings. The core challenge was integrating decision support into a workflow where interaction opportunities are extremely limited and errors carry clinical risk.
Core Design Question
“How can a decision support system operate inside a live endoscopy room without increasing cognitive load, procedure time, or error risk?”
Understanding the Environment
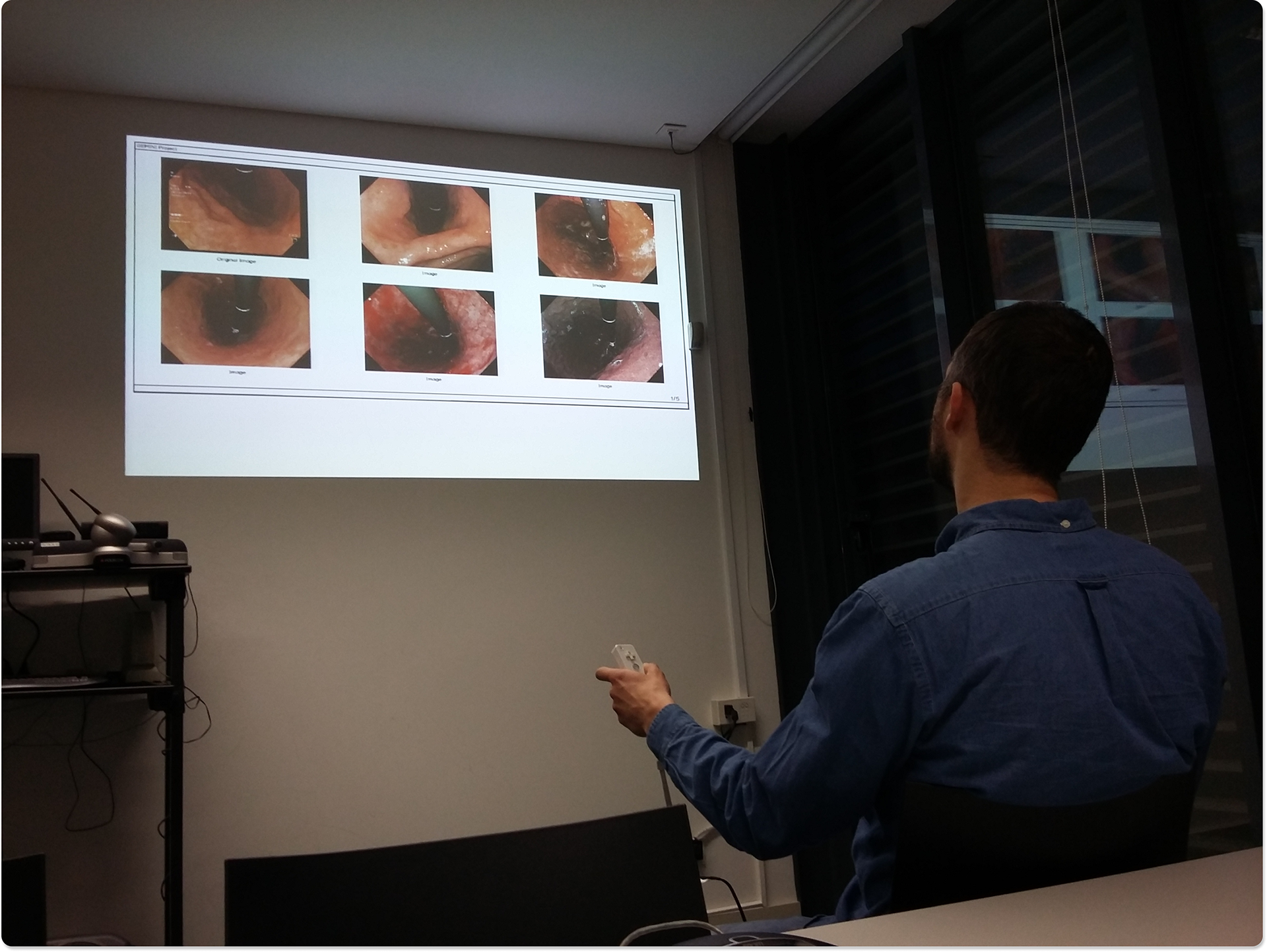
To ground the work in reality, ethnographic studies were conducted inside gastroenterology exam rooms:
• Observing full endoscopic procedures to understand attention flow, timing, and physical constraints
• Conducting contextual interviews with doctors, nurses, auxiliary staff, and patients
• Modeling personas based on procedural roles
• Identifying moments where interaction was feasible or not
This work clarified that any successful solution would need to minimize interaction, avoid visual distraction, and fit seamlessly into existing routines.
Exploring Interaction Paradigms
Four interaction paradigms were explored (voice, gesture, touch, endoscope-based interaction) and evaluated against clinical constraints.
Medium-fidelity prototypes were created for each paradigm and tested both on-site with clinicians and off-site with medical students. Two usability testing cycles, paired with expert review, were sufficient to converge on a final interaction model that minimized disruption to clinical workflows while remaining learnable and reliable.
Supporting Systems
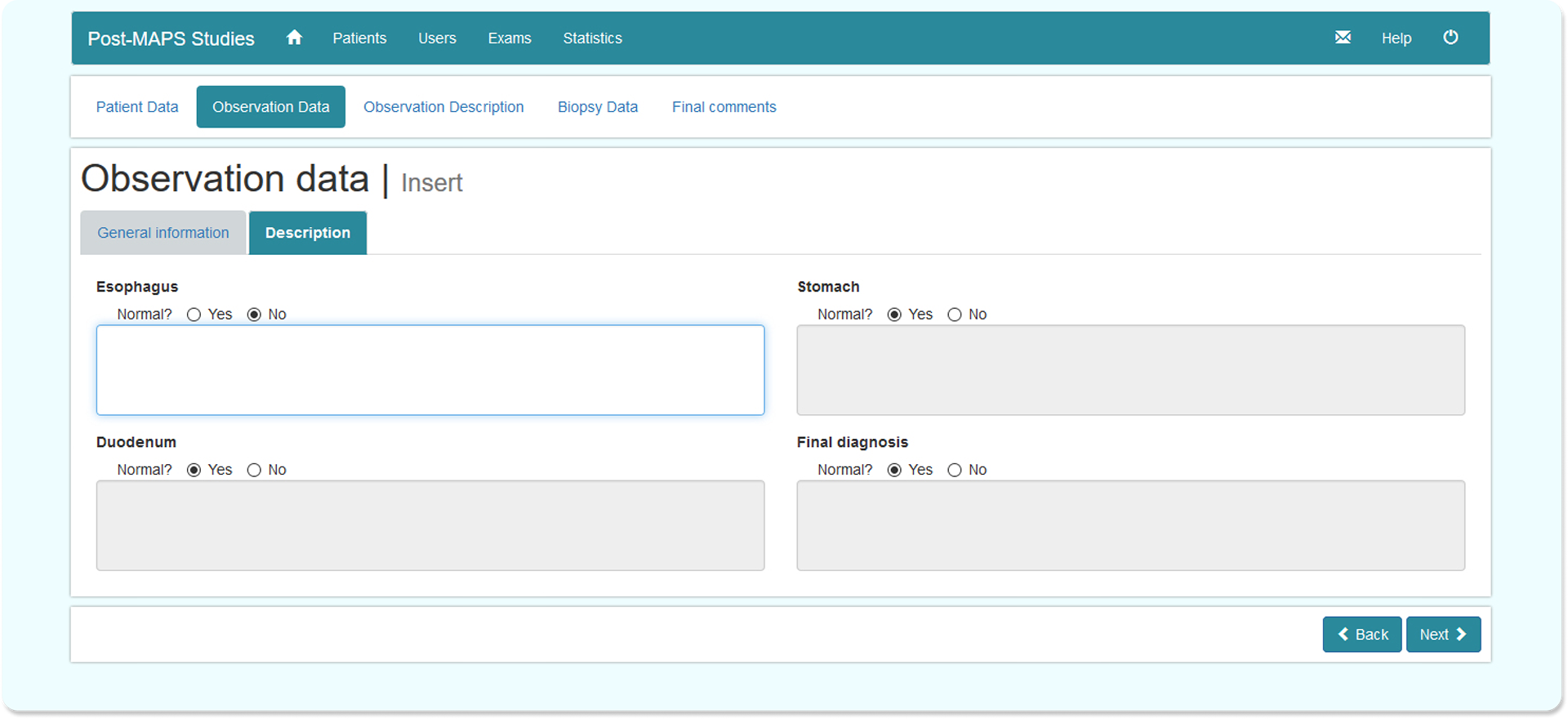
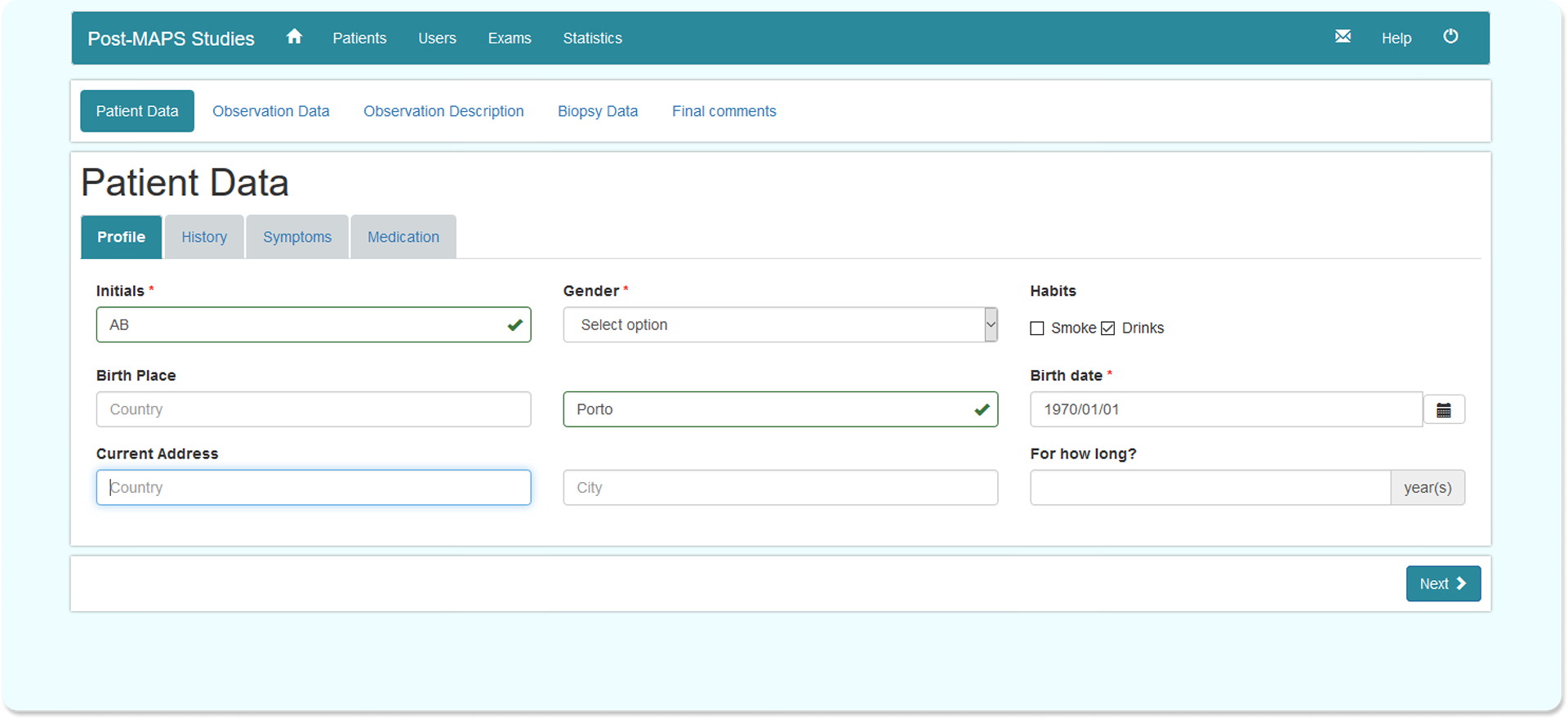
In parallel, a web-based platform was designed to support the clinical protocol by enabling structured collection of patient and observation data across multiple European medical centers. Requirements were derived from interviews with clinical staff and translated into use cases, user flows, and a simple, objective information architecture. Dogfooding sessions were used to identify usability issues and edge cases before releasing a stable version.
Design priorities included:
• Wizard-based data entry reflecting non-negotiable protocol steps
• Strong content strategy to prevent incomplete or ambiguous records
• Clear step-by-step guidance and immediate feedback
• Explicit error recovery paths to reduce data loss and entry mistakes
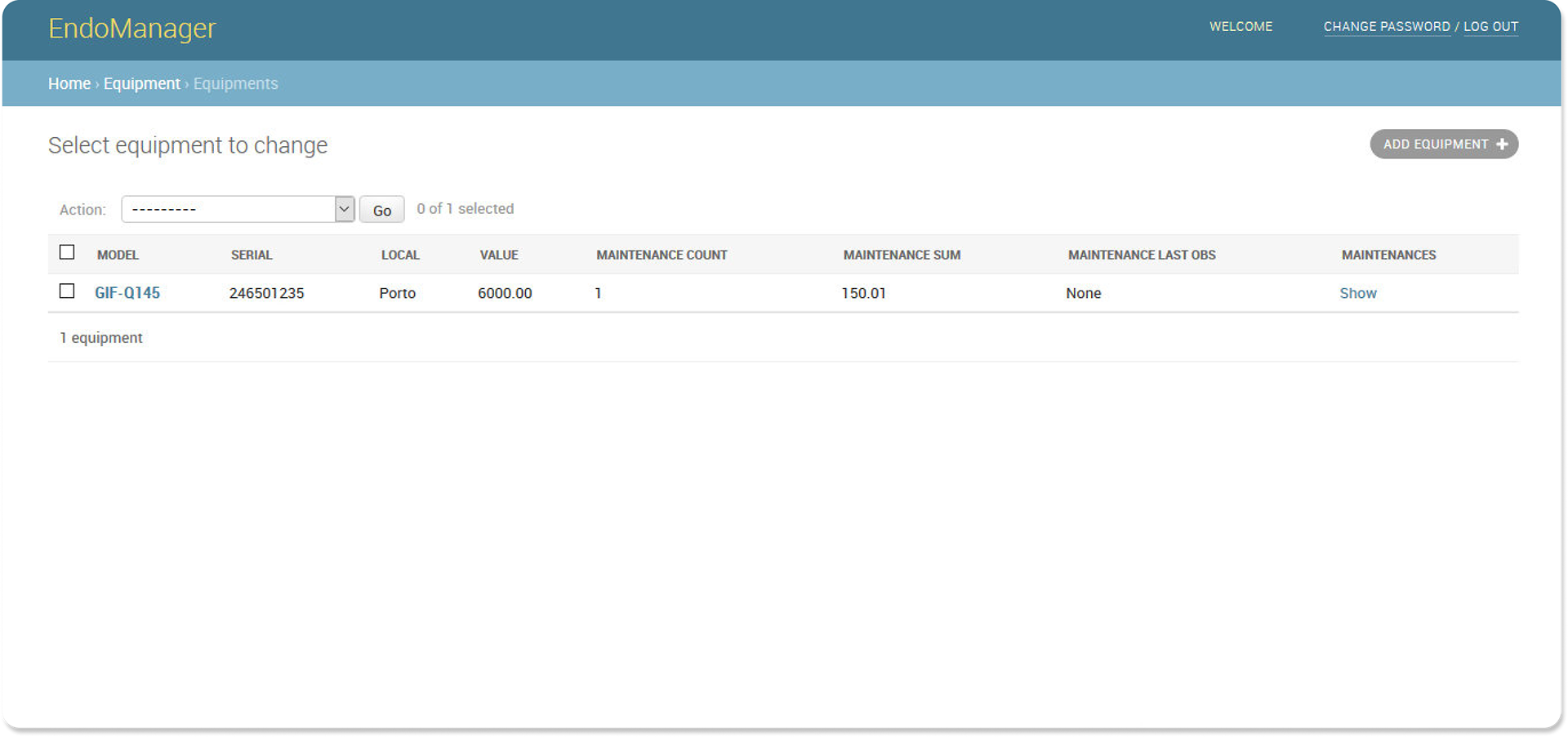
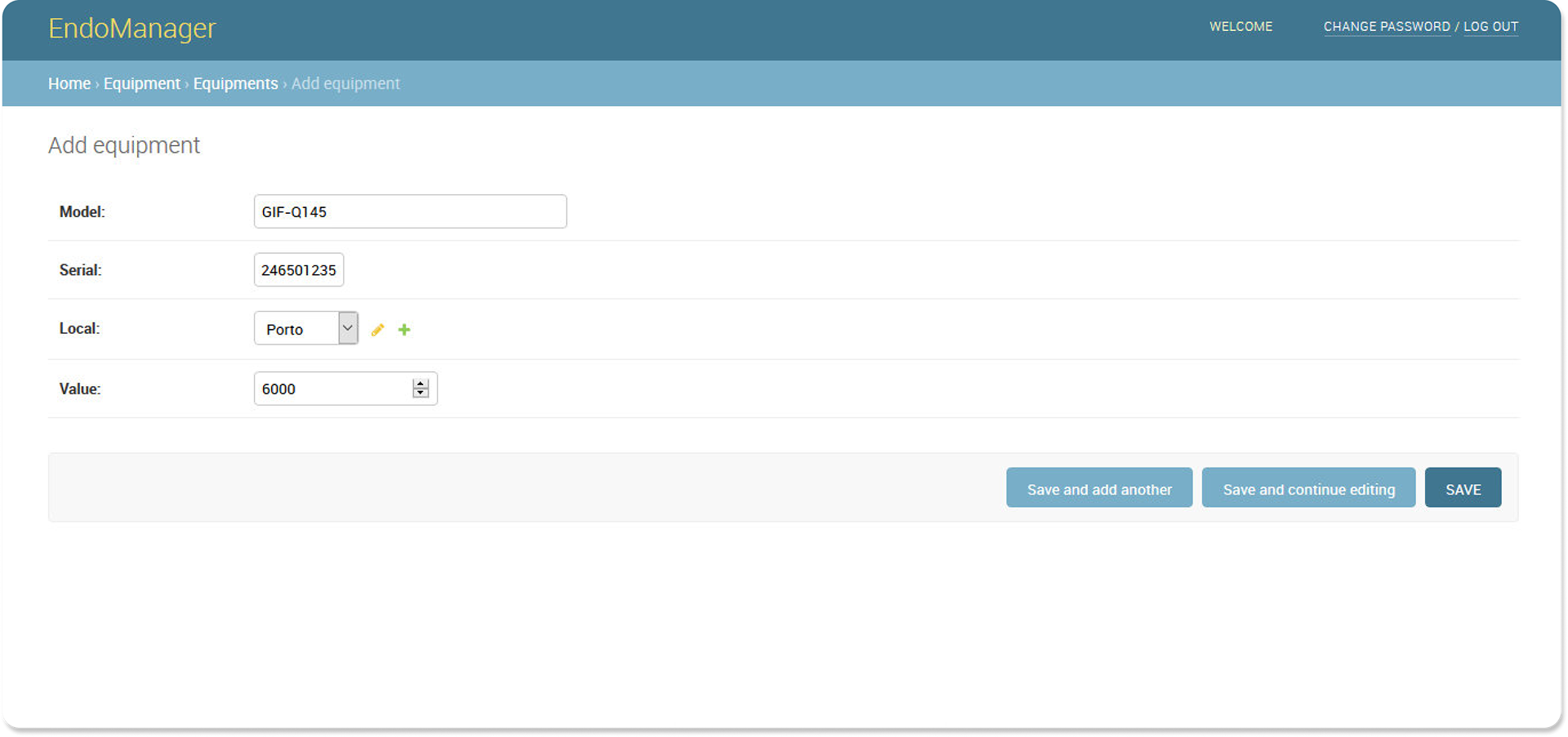
A smaller project involved the design of an endoscope maintenance management tool. Features and content were defined through close participatory design with technicians, and the final system was delivered for in-house use.
Outcomes and Impact
• Web-based clinical data platform deployed across multiple European medical centers
• Clinical decision support system validated for use during live endoscopic procedures
• Systems used in real clinical environments for 2+ years with no major usability incidents
• Supported a validated diagnostic protocol (earning the Pfizer Research Award 2016)
• Contributed to three peer-reviewed scientific publications